Ensure you remain healthy with a colonoscopy
Did you know that 1 in every 20 adult Americans will develop colon cancer in his or her lifetime? Early detection and the removal of all colon polyps is the best method for fighting this condition.
The most effective way to detect and treat this cancer is with a colonoscopy. Today, this procedure is considered safe, simple, and extremely effective.
If you have had polyps, colitis, or colon cancer in the past, a colonoscopy is also an effective tool for monitoring patients to ensure the cancer doesn't grow back.
When should I get a colonoscopy?
- Changes in bowel habits
- Blood in your stool
- An unusual abdominal pain
- A history of colon polyps in your family
- A history of colon cancer in your family
- Suffering from inflammatory bowel disease
- Suffering from Crohn’s disease
Frequently asked questions:
Q. What is a colonoscopy?
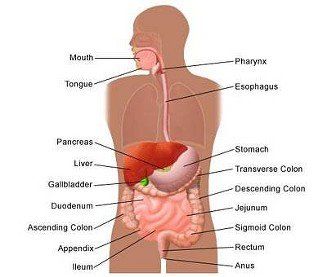
A. The colon, which is shaped like a very large question mark with many twists and turns, begins in the right lower abdomen and ends in the rectum. A colonoscopy is a safe, effective method of visually examining the colon using a very narrow lighted, flexible fiber optic tube called a colonoscope. At the end of the tube is a miniature camera with a wide-angle lens that helps your doctor examine the lining of your digestive tract on a video monitor. More accurate than a barium enema X-ray and much simpler than exploratory abdominal surgery, colonoscopy is safe and generally well-tolerated by patients.
Q. How do I know if I need a colonoscopy?
A. Your physician may recommend a colonoscopy if you have changes in bowel habits, blood in your stool, an unusual abdominal pain, a history of colon polyps or a history of colon cancer in your family, or if you suffer from inflammatory bowel disease (colitis) or Crohn’s disease. Colonoscopies also can verify findings of polyps or tumors located with a barium enema exam, as well as evaluate intestinal inflammation, ulcerations and diverticulitis.
Q. What should I do before the procedure?
A. Always tell your doctor if you are taking any medications – particularly those that may affect blood clotting — or if you have any special medical conditions, including diabetes, pregnancy, lung or heart conditions. Also let your doctor know if you are allergic to any medications. If you have ever been told to take antibiotics before a dental or surgical procedure, you may need to take antibiotics before a colonoscopy. Your physician can answer all your questions.
Q. Is any preparation necessary before the procedure?
A. Yes. Your colon must be completely empty for the colonoscopy to be thorough and safe. There are a variety of preparations your doctor can choose from to flush the colon, including tablets or a liquid solution that you drink. In addition, you will be asked to drink only clear liquids for one or two days before the procedure and you will be given advice on taking regular medications during that time. A list of detailed instructions will be provided by your physician.
Q. What happens during the procedure?
A. On the day of the procedure you will be given a mild sedative to help you relax. During the procedure, you will lie on your left side on an examining table and the physician will insert the colonoscope into the rectum and gently move it through your colon. There are several tiny instruments in the scope that help the physician during the procedure: one to blow air into your colon, which inflates it to help the physician see better; one to remove polyps or take biopsies; and one to stop any bleeding. After the procedure, you may experience a little discomfort, like the feeling of having gas, but that soon subsides. The entire procedure usually takes less than 30 minutes and most people can resume their regular diet later that day.
Q. What happens after the examination?
A. Your physician will explain the findings to you. If a biopsy was performed or a polyp removed, you should get the results in about a week. Your physician may give you other special instructions as well. Even though you should feel fine, you must have someone else drive you home after the procedure because of the sedatives. You should not drive, operate heavy machinery or make important decisions for up to six hours after your procedure.
If you’ve had prolonged effects from the sedative, you may need to make a follow-up appointment. If you have excessive or prolonged rectal bleeding or severe abdominal pain, fever or chills, call your doctor right away.
Q. Are there any risks associated with having a colonoscopy?
A. Serious complications from this procedure are very rare. Of course, as with any medical procedure, they can occur. Complications might include excessive bleeding, especially if a large polyp was removed, or, in rare cases, a tear in the lining of the colon, which might require hospitalization or surgery. Again, these complications are rare.
Q. What is Fuse™?
A. Fuse™, or ‘full spectrum endoscopy,’ is the latest advancement in colon cancer screenings and endoscope technology used in colonoscopy and upper GI endoscopy. It allows the physician a 330-degree field of view during the procedure.
Q. Will the procedure or my risks be any different if my physician uses Fuse™ technology?
A.
As a patient, your prep and your experience during the procedure, as well as any potential risks, are exactly the same as if your physician used a traditional endoscope. The difference with Fuse endoscopes is experienced by the physician, not the patient.
Receive optimal care here at Southland Gastroenterology Medical Group Inc
A colonoscopy is much more effective than a barium enema X-ray and much simpler than exploratory abdominal surgery. Make sure you stay healthy with our advanced detection procedures.
Call the physicians here at Southland Gastroenterology Medical Group Inc to make an appointment.
Hemet
951-929-1177
Murrieta
951-672-7885
Sun City
951-304-3900